
menu


There are a variety of sores that can occur in or around the mouth. Most are benign, but some may be indicative of cancer.
These small, creamy white ulcers have a red border and always appear inside the mouth. Canker sores can be painful, but they are not contagious. They usually heal in one-to-two weeks. Prescription drugs and over-the-counter topical treatments can help reduce the pain.
Also known as fever blisters, cold sores are fluid-filled blisters that form on the lips or around the mouth. Cold sores are usually caused by the Herpes Simplex Virus, and are both contagious and painful. Fever, sunburn, trauma, hormonal changes or emotional upset can trigger their appearance. While there is currently no cure, cold sores can be treated with prescription ointments to help alleviate the pain. It is also important to wash your hands frequently and avoid sharing personal products to help prevent the spread of the infection to other people.
Also known as oral thrush, this mouth sore is caused by a fungal infection. Painful red and cream-colored patches form on moist areas of the mouth. Candidiasis can cause difficulties with swallowing and taste. It is most commonly seen by denture wearers or people who have problems with their immune systems. Sometimes it occurs as a result of an unrelated antibiotic treatment, which can decrease normal bacterial development in the mouth. Saliva substitutes and antifungal creams are used to treat candidiasis.
Chronic irritations inside the mouth, such as cheek chewing, dentures or braces, sometimes cause benign white patches to form inside the mouth. The treatment is to alleviate the irritation to allow for natural healing.
Leukoplakias consist of thick, white lesions that most commonly form beneath or around the tongue, cheeks or gums. Leukoplakias are painless, but can become cancerous over time. These mouth sores are most often seen in tobacco users. A biopsy may be needed to accurately diagnose leukoplakias.
If you have a mouth sore that won’t heal, please contact our office and schedule an appointment with one of our Otolaryngologists.
Everyone experiences sore throats when they have a cold or flu. But there are other reasons for sore throats that may be symptomatic of more serious problems.
Strep throat is caused by streptococcal bacteria (strep) in the throat and often the tonsils. Symptoms include sudden severe sore throat, pain swallowing, a fever over 101F, swollen tonsils and lymph nodes, and white or yellow spots on a reddened back of the throat. Strep throat is highly contagious, with a two-to-five day incubation period. It can be diagnosed through a physical examination and a throat culture. Strep throat is treated with antibiotics and usually resolves in three to seven days, although the healing time can be up to two weeks. It is important to have strep throat diagnosed and begin treatment as soon as possible in order to prevent its spread to others.
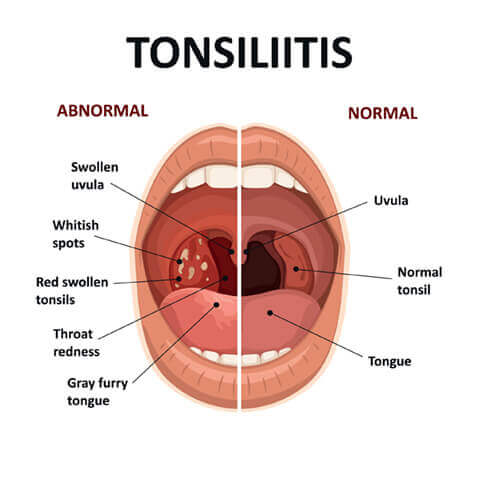
Tonsillitis is an inflammation of the tonsils located in the back of the throat on both sides of the tongue. Tonsils are part of the body’s natural immune system. This tissue captures bacteria and viruses to either prevent them from entering the body or trigger the appropriate immune response. The back of the throat may appear red or swollen or have a white or yellow coating covering the tonsils. The adenoids (tissue high in the throat behind the nose and soft palate) may also be inflamed and swollen, impeding swallowing and/or breathing. Symptoms include a severe sore throat, painful or difficult swallowing, coughing, headache, fever, chills and swelling of the cheeks and neck. Tonsillitis may also be caused by strep throat. Antibiotic medication is generally prescribed to treat the inflammation. Tonsillitis usually resolves in four to seven days if caused by a virus. Chronic cases of repeated tonsillitis may require surgical removal of the tonsils and/or adenoids (tonsillectomy and adenoidectomy). An adenoidectomy may also be recommended for children experiencing chronic ear infections.
If you would like to learn more about your tonsils please visit mytonsils.com.
The larynx allows air to pass in and out of the lungs while preventing solids (food) and liquids from entering the lungs. The larynx also contributes to sound production by the vocal cords. Laryngitis is an inflammation of the larynx, the top portion of the windpipe (trachea). It is characterized by hoarseness, coughing, difficulty in breathing for some children and, occasionally, loss of voice. In addition to an infection, laryngitis may be caused by acid reflux, nodules, polyps or nerve damage on the vocal cords. Laryngitis usually heals by itself within two weeks with the help of increased air moisture, drinking plenty of fluids and resting the voice.
The pharynx is tissue that resides behind the mouth and soft palate and acts as a pathway for food and liquids to enter the esophagus and air to enter the lungs. An inflammation of the pharynx is called pharyngitis. Painful swallowing is the most common symptom. Pharyngitis may also occur along with laryngitis. Again, the inflammation usually heals by itself with rest, fluids and air humidity.
The epiglottis is a flap of tissue at the base of the tongue that keeps food from going into the windpipe when swallowing. Epiglottitis occurs when this tissue becomes inflamed and infected. The swelling of the epiglottis can block the tongue and result in a medical emergency. In addition to infections, epiglottitis can be caused by chemicals, severe heat damage, or trauma.
If you experience a sore throat that hampers your ability to swallow, seek immediate medical attention. If you have a sore throat that causes pain or won’t heal, please contact our office and schedule an appointment with one of our Otolaryngologists.
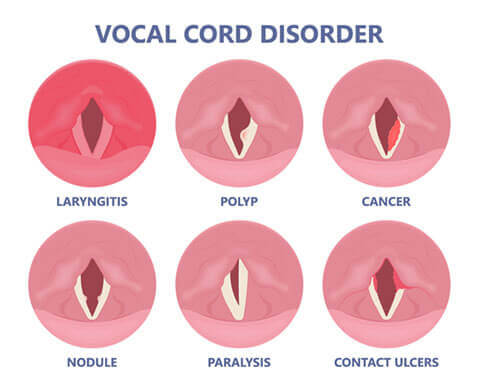
Abnormal changes in the voice are called “hoarseness.” When hoarse, the voice may sound breathy, raspy, strained, or show changes in volume or pitch (depending on how high or low the voice is). Voice changes are related to disorders in the sound-producing parts (vocal folds) of the voice box (larynx). While breathing, the vocal folds remain apart. When speaking or singing, they come together and, as air leaves the lungs, they vibrate, producing sound. Swelling or lumps on the vocal folds hinder vibration, altering voice quality, volume, and pitch.
Acute Laryngitis: The most common cause is acute laryngitis— (swelling of the vocal folds) that occurs during a common cold, upper respiratory tract viral infection, or from voice strain. Serious injury to the vocal folds can result from strenuous voice use during an episode of acute laryngitis.
Voice Misuse: Speaking in noisy situations, excessive use, telephone use with the handset cradled to the shoulder, using inappropriate pitch (too high or too low) when speaking, not using amplification when public speaking.
Benign Vocal Cord Lesions: Prolonged hoarseness can occur when you use your voice too much, or too loudly for extended periods of time. These habits can lead to nodules, polyps, and cysts. Vocal nodules (singers’ nodes) are callus-like growths of the vocal folds. Vocal fold polyps and cysts also occur in those who misuse their voice, but can also occur in those who do not.
Vocal Hemorrhage: If you experience a sudden loss of voice following a yell or other strenuous vocal use, you may have developed a vocal fold hemorrhage. Vocal fold hemorrhage occurs when one of the blood vessels on the surface of the vocal folds ruptures and the soft tissues fill with blood. It is considered a vocal emergency and should be treated with absolute voice rest and examination by an Otolaryngologist (Ear, Nose, and Throat doctor).
Gastroesophageal Reflux (GERD): A possible cause of hoarseness is gastro-esophageal reflux, when stomach acid comes up the swallowing tube (esophagus) and irritates the vocal folds. Other typical symptoms of GERD include heartburn and regurgitation. Usually, the voice is worse in the morning and improves during the day. These people may have a sensation of a lump or mucus in their throat and have an excessive desire to clear it.
Laryngopharyngeal Reflux (LPRD): If the reflux makes it all the way up through the upper sphincter and into the back of the throat, it is called LPRD rather than GERD. The structures in the throat (pharynx, larynx, and lungs) are much more sensitive to stomach acid and digestive enzymes, so smaller amounts of the reflux into this area can result in more damage. Many patients with LPRD do not have heartburn or other classic symptoms of GERD. It is often referred to as “Silent Reflux”.
Smoking: Smoking is another cause of hoarseness. Because smoking is the major cause of throat cancer, if smokers become hoarse, they should see an Otolaryngologist.
Neurological Diseases or Disorders: Hoarseness can also appear in those who have neurological diseases such as Parkinson’s or a stroke, or may be a symptom of spasmodic dysphonia, a rare neurological disorder that usually affects only the voice, but sometimes affects breathing. A paralyzed vocal fold may be the cause of a weak, breathy voice. If the hoarseness persists for more than three months and other causes have been ruled out, a neurologist may be helpful for diagnosis.
Other Causes: These include allergies, thyroid problems, trauma to the voice box, and, occasionally, menstruation. Very serious conditions such as laryngeal cancer can also cause hoarseness, which is why it is important to have chronic hoarseness evaluated promptly by an Otolaryngologist.
Hoarseness caused by a cold or flu may be evaluated by family physicians, pediatricians, and internists who have learned how to examine the larynx. Problems with the voice are often best managed by a team of professionals who know and understand how the voice functions. These professionals are Otolaryngologists, Speech/Language Pathologists, and teachers of singing, acting, and public speaking. Vocal nodules, polyps, and cysts are typically treated with a combination of microsurgery and voice therapy.
Otolaryngologists will obtain a thorough history of a patient’s hoarseness and general health. They will then evaluate the voice and do a complete ear, nose, and throat exam. This includes examination of the vocal folds by laryngoscopy. Laryngoscopy may be suggested by the Otolaryngologist at any time during an evaluation for hoarseness, but if it persists beyond three weeks it should be evaluated and that evaluation should occur within a maximum of 3 months. The evaluation should be immediate if there is concern about a serious underlying cause is suspected.
Doctors usually look at the vocal folds either with a mirror placed in the back of the throat, or with a very small, lighted flexible tube (fiberoptic scope) that is passed through the nose to view the vocal folds. Videotaping or stroboscopy (slow-motion assessment) may also help with the analysis. These procedures are well tolerated by most patients. In some cases, special tests designed to evaluate the voice may be recommended. These measure voice irregularities, how the voice sounds, airflow, and other characteristics that are helpful in diagnosing and guiding treatment.
The treatment of hoarseness depends on the cause. Many common causes of hoarseness can be treated simply by resting the voice or modifying how it is used. An Otolaryngologist may make some recommendations about voice use behavior, refer the patient to other voice team members, and in some instances recommend surgery if a lesion, such as a polyp, is identified. Not smoking and avoiding secondhand smoke is recommended to all patients. Drinking fluids and taking medications to thin out the mucus may help.
Specialists in speech/language pathology (voice therapists) are trained to assist patients in behavior modification to help eliminate some voice disorders. Patients who have developed bad habits, such as smoking or overusing their voice by yelling and screaming, benefit most from this conservative approach. The Speech/Language Pathologist may teach patients to alter their methods of speech production to improve the sound of the voice and to resolve problems, such as vocal nodules. When a patient’s problem is specifically related to singing, a singing teacher may help to improve the patients’ singing techniques.
Please see Laryngoscopy under Treatments for more information.

The ear is made up of three sections: the outer ear, middle ear and inner ear. Each of these areas is susceptible to infections, which can be painful. Young children have a greater tendency to get earaches. While most ear pain resolves itself in a matter of days, you should get a physical examination to understand the type of infection, prevent it from spreading and obtain treatment to help alleviate the pain.
Also known as Swimmer’s Ear, outer ear infections result from an inflammation, often bacterial, in the outer ear. Generally, they happen when water, sand or dirt gets into the ear canal. Moisture in the air or swimming makes the ear more susceptible to this type of ear infection. Symptoms include: severe pain, itching, redness and swelling in the outer ear. There also may be some fluid drainage. Often the pain is worse when chewing or when you pull on the ear. To reduce pain and prevent other long-term effects on the ear, be sure to see a doctor. Complications from untreated otitis externa may include hearing loss, recurring ear infections and bone and cartilage damage. Typically, your doctor will prescribe eardrops that block bacterial growth. In more severe cases, your doctor may also prescribe an antibiotic and pain medication. Most outer ear infections resolve in seven to 10 days.
Middle ear infections can be caused by either bacterial or viral infection. These infections may be triggered by airborne or foodborne allergies, infections elsewhere in the body, nutritional deficiencies or a blocked eustachian tube. In chronic cases, a thick, glue-like fluid may be discharged from the middle ear. Treatment is contingent on the cause of the infection and ranges from analgesic eardrops, medications, to the surgical insertion of a tube to drain fluid from the middle ear or an adenoidectomy.
Also known as labyrinthitis, inner ear infections are most commonly caused by other infections in the body, particularly sinus, throat or tooth infections. Symptoms include dizziness, fever, nausea, vomiting, hearing loss and tinnitus. Always seek medical attention if you think you may have an inner ear infection.
If you suspect you or your child may have an ear infection, please contact our office and schedule an appointment with one of our Otolaryngologists.
The inner ear serves two purposes: hearing and balance. There are mechanisms in the ear that inform the brain about your position, orientation in space and movement and all times to keep you in balance. A false sensation of spinning or whirling, known as vertigo, can occur when the signal to the brain is blocked or misfires. In addition to the sensation of dizziness, symptoms may include headache, nausea, sensitivity to bright light, blurred vision, ringing in the ears, ear pain, facial numbness, eye pain, motion sickness, confused thinking, fainting and clumsiness.
Dizziness can also be a symptom of a more serious medical problem, such as high or low blood pressure, heart problems, stroke, tumor, medication side effect or metabolic disorders. Therefore you should always seek medical attention if you experience ongoing or repetitive dizziness.
An Acoustic Neuroma is a benign growth on the nerve that connects the inner ear to the brain. An MRI is ordered to diagnose this tumor, especially if the hearing is asymmetric between the ears.
BPPV occurs when tiny calcium crystals in the ears loosen and begin moving about the wrong part of the ear. It is characterized by sudden, short bursts of dizziness that happen most often as a result of head movement. There is no known cause for BPPV. It usually resolves itself in a matter of days, but can also be improved by an Epley Maneuver (a repositioning) that your doctor can do in the office.
Dizziness may be one symptom of an inner ear infection. Typically this is due to a viral upper respiratory infection (viral neuritis) and can sometimes also affect hearing (labyrinthitis). Sometimes steroids are prescribed to decrease the inflammation which should then improve the symptoms of dizziness and/or hearing loss.
Meniere’s Disease is characterized by long periods of dizziness, lasting from 30 to 60 minutes or more. It is accompanied by symptoms such as ringing in the ears, hearing loss and a feeling of fullness in the ear. There is no known cause or cure for Meniere’s Disease, although medication and behavior changes can help reduce the severity of the symptoms.
Some migraines (vestibular migraines) can cause a feeling of imbalance and vertigo. This may be accompanied by sensitivity to light and/or sound, ringing in the ears or hearing loss. Migraine-related vertigo may occur in conjunction with or separate from the migraine headache.
If you’re experiencing any form of repetitive or chronic dizziness, please contact our office and schedule an appointment with one of our Otolaryngologists.